Hospital-Acquired Infections
Hospital Acquired Infection Lawyer
Hospital Acquired Infections
A hospital acquired infection is any infection you get while in the hospital that has nothing to do with the condition that brought you to the hospital in the first place. Throughout my 40+ year career as a medical malpractice lawyer, I’ve seen this happen far too often. If you went to the hospital for a procedure, and left with surgical site infection due to instruments left within you, or ventilator associated pneumonia, or other infection, you need to call me! I’ll Make Them Pay!®
The most common hospital acquired infections include:
Bloodstream Infections
Infections in the blood stream are extremely dangerous because they affect the functions of your entire body. Examples include:
1. HIV (human immunodeficiency virus)– a virus that attacks and weakens the body’s immune system, making individuals more susceptible to infections and diseases.
2. Hepatitis– a condition characterized by inflammation of the liver, often caused by viral infections.
3. AIDS-AIDS (acquired immunodeficiency syndrome) is the late stage of HIV infection. It occurs when the immune system is severely due to the virus. People with AIDS are highly vulnerable to various infections and diseases due to the weakened immune system.
4. Bacterial– A bacterial bloodstream infection, also known as bacteremia, occurs when bacteria enter the bloodstream and spread throughout the body. It is a severe condition that can lead to serious complications like sepsis.
Urinary Tract Infections
Infections in the urinary tract can lead to even more dangerous infections in the bladder and kidneys. Without proper treatment, urinary tract infections can lead to permanent kidney damage.
Respiratory Infections
Influenza (Flu): Influenza is a viral respiratory infection that can cause symptoms such as fever, cough, sore throat, body aches, and fatigue. It is typically spread through respiratory droplets from infected individuals and can have seasonal outbreaks.
Pneumonia: Pneumonia is an infection that causes inflammation in the lungs. It can be caused by various pathogens, including bacteria, viruses, or fungi (all very prevalent in hospitals). This is a common type of hospital infection, which is why it is so important for proper cleaning protocols to be followed. Symptoms of pneumonia may include cough, difficulty breathing, chest pain, fever, and fatigue. Pneumonia can range from mild to severe, and treatment depends on the underlying cause.
Tuberculosis (TB): Tuberculosis is a bacterial lung disease caused by Mycobacterium tuberculosis. It can be transmitted through the air when an infected individual coughs or sneezes. Symptoms may include persistent cough, chest pain, fatigue, weight loss, and night sweats.
Bronchitis: Bronchitis is an inflammation of the bronchial tubes, which are the air passages that connect the lungs to the throat. It can be caused by viral or bacterial infections. Symptoms may include cough with mucus, chest discomfort, shortness of breath, and mild fever. Most cases of bronchitis resolve on their own, but treatment may be necessary for severe or persistent cases.
Pneumonia: an inflammation and fluid in the lungs. Elderly and young children are at the greatest risk of pneumonia, which if not treated properly, can lead to death.
Severe Acute Respiratory Syndrome (SARS): A viral respiratory illness caused by a coronavirus. It was first identified in 2003 and can cause symptoms such as fever, headache, body aches, and a dry cough. SARS can be transmitted through close person-to-person contact, particularly through respiratory droplets.
It is vitally important that hospital staff maintains cleanliness throughout the building to avoid a hospital acquired infection for each patient. Medical professionals also need to be diligent in cleaning their hands between patient visits. Hospital infection lawyers work to make sure cleanliness standards are upheld! If you have suffered because an infection occurred as a result of improper santiization during a hospital stay, I’ll Make Them Pay!®
Surgical Site Infections (SSI)
Surgical site infections can occur because of dirty surgical equipment, left-behind tools, improperly washed hands. Common surgeries that can lead to infection are implantation of hardware for various reconstructive surgeries, including knee replacements and spinal rods. Infections include:
Superficial Incisional SSI: This type of SSI affects the skin and subcutaneous tissue near the surgical incision. It may manifest as redness, warmth, tenderness, delayed healing, and sometimes the presence of pus at the wound site.
Deep Incisional SSI: Deep incisional SSIs involve tissues beneath the skin, such as muscles or organs near the surgical site. Symptoms may include fever, pain, swelling, drainage of pus, and the wound splitting open.
Organ/Space SSI: This type of SSI affects any part of the body other than the incision site, such as an organ or the abdominal cavity. It can be more severe and may present with systemic symptoms, such as fever, pain, abscess formation, and pus in the affected area.
Wound Dehiscence: Although not specifically an infection, wound dehiscence refers to the separation or opening of a surgical incision. It can be a result of poor wound healing and may increase the risk of infection by exposing the underlying tissues.
Necrotizing Fasciitis: This is a rare but severe type of SSI characterized by rapid, progressive infection of the skin, subcutaneous tissue, and fascia. It can cause severe pain, redness, swelling, and tissue destruction. Necrotizing fasciitis requires immediate medical attention and surgical intervention.
Staph Infections
MRSA is the most common staph infection. It is incredibly dangerous and contagious because of it’s resistance to antibiotics.
Causes Of Hospital Acquired Infections
While many hospital acquired infections cannot be prevented, it is still a health care facility’s responsibility to provide patients with the safest environment possible. Whether you’ve suffered from one of these infections or find yourself at risk of acquiring one, it is important to know how they are caused.
Avoid the causes of hospital-acquired infections, or make sure to protect yourself as much as you can in these situations, might save your life:
Overuse or improper use of antibiotics
The overuse or improper use of antibiotics can contribute to the development of antibiotic-resistant bacteria, also known as multidrug-resistant organisms. These bacteria have evolved to withstand the effects of antibiotics, making them more difficult to treat.
Injections
If proper aseptic techniques are not followed during the injection process, bacteria or other pathogens can be introduced into the body, potentially causing an infection.
Surgical procedures
Despite maintaining a sterile environment, there is a possibility of contamination during the surgical procedure. This can occur through contact with the patient’s own skin or bodily fluids, healthcare personnel, surgical instruments, or the surrounding environment. If the introduced microorganisms are not adequately controlled, they can cause an infection.
Exposure to hospital personnel
Hospital personnel, such as doctors, nurses, or other healthcare workers, may come into direct contact with infected patients or contaminated surfaces, instruments, or equipment. If proper hand hygiene practices are not followed, the microorganisms present on the hands of healthcare personnel can be transmitted to patients, leading to infections.
Inadequate hand washing
The hands of healthcare workers are a primary source of transmitting infectious agents responsible for infection. If the hospital staff does not practice proper hand hygiene, they can carry and spread harmful microorganisms from one patient to another. The healthcare workers can also contaminate surfaces, medical equipment, or other healthcare settings.
Lengthy hospital stays
Extended hospital stays mean patients have prolonged exposure to various microorganisms present in healthcare settings. Hospitals can be reservoirs of infectious agents, and the longer a patient stays, the higher the likelihood of coming into contact with potentially harmful bacteria, viruses, or fungi.
Exposure to unclean equipment
Transmission of pathogens: Dirty equipment, such as contaminated medical devices, surfaces, or instruments, can harbor and transmit pathogens responsible for infections. Bacteria and viruses can survive on surfaces and equipment, and if proper cleaning and disinfection protocols are not followed, they can be transferred to patients, leading to infections.
Cross-contamination: When impure equipment comes into contact with patients or healthcare providers, it can act as a source of cross-contamination. For example, if a contaminated instrument is used on multiple patients without proper cleaning and sterilization between uses. This can introduce pathogens from one patient to another, increasing the risk of infections.
Reservoirs for infectious agents: Unclean equipment can serve as reservoirs for infectious agents, providing a favorable environment for their survival and proliferation. This can include equipment with hard-to-reach areas that are difficult to clean thoroughly or devices that have complex mechanisms where pathogens can hide and persist. If these reservoirs are not properly addressed, they can serve as a continuous source of infection.
Exposure to others with hospital-acquired infections
Hospital acquired infections can spread from one patient to another through direct contact or close proximity. This can occur when infected patients cough, sneeze, talk, or touch surfaces without proper hand hygiene. Pathogens, such as bacteria or viruses, can be released into the air or deposited on surfaces, increasing the risk of transmission to other patients.
Hospital Acquired Infection Could Be Medical Malpractice
When a patient acquires an infection during their hospital stay, there are circumstances where the hospital can be sued for medical malpractice. To establish a medical malpractice claim in this scenario, the following elements generally need to be proven:
Duty of care: The hospital must have owed a duty of care to the patient. This means they had a legal obligation to provide a certain standard of care and take reasonable measures to prevent infections.
Breach of duty: It must be demonstrated that the hospital breached its duty of care by failing to adhere to acceptable standards of infection prevention and control. Thereby increasing the risk of the patient acquiring the infection.
Causation: The patient needs to establish that the hospital’s breach of duty was the direct cause of their infection. This requires showing that the infection was acquired as a result of the hospital’s negligence and not due to other factors unrelated to the hospital’s actions.
Damages: The patient must demonstrate that they suffered harm or damages as a result of the acquired infection. This can include physical injuries, pain and suffering, medical expenses, loss of income, and other related losses.
Proving a hospital’s liability for a patient-acquired infection can be complex, as it requires establishing negligence on the part of the hospital. Then a causal link between the negligence and the infection must be show by the patient. It may involve gathering medical records, expert testimony, and other evidence to support the claim. Each case is unique, and the outcome will depend on the specific facts and circumstances surrounding the infection and the hospital’s actions.
If you or someone you love was injured as the result of a hospital-acquired infection, you have to call me now for a FREE consultation. I will help you understand your rights. As your Ohio Medical Malpractice Lawyer, I’ll be there for you, and I’ll Make Them Pay!®
ASK TIM A QUESTION
NO COST TO YOU!
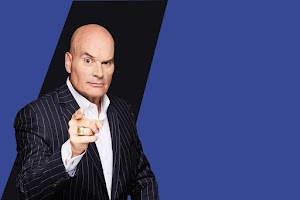
There's the Tim Misny you see on the billboards and on TV, but there's another Tim Misny that I know up close and personal.
The Tim Misny I know is genuinely passionate about helping the hard working little folks who get pushed around the big folks. He actually, really honestly cares about people who run into bad luck at no fault of their own. Tim has quietly, out of the sight of cameras and with no fanfare shared generously with the marginalized in our society; single moms, Veterans and others without expecting anything in return.
He calls them like he sees them and you wouldn't want to take your troubles to anyone else.
Thank you Tim for being a light in this community!
City, State and Above State Level Situation .
Pro Se !
Thank you Tim
father figure one day. Tim loves nature & shares the true beauty of nature with how he raises his kids. From biking through trails & having his kids learn how to nurture the family garden - he teaches valuable lessons on how to appreciate the world we live in. I know that Tim is just a phone call away & always urgent to responding no matter the situation. He has given me some of the greatest advice & continously throwing positive energy my way! I'm honored to know him & be a friend of his. He is the true practioneer of changing lives & paying it forward. He has taught me so much in just a short amount of time. Tim Misny, a man that wakes up every single day to make a difference!

After I helped him through the checkout and he left, many different employees at the garden center asked me if I knew who that man was. I did not. They told me, “That’s Tim Misny!” Once I figured out “who” Tim Misny was, my confidence grew. It was a pivotal moment. One in which steered the rest of my life. His words stuck with me. I worked hard and obtained my Associate’s Degree in Criminal Justice. I was hired by a local Law Enforcement Agency at the age of 21. I was sent to the Ohio State Highway Patrol Academy, which was an extremely tough place to be, to say the least. At the Academy, they try to break those who don’t have a determined spirit. On days I wanted to quit, I remembered Tim’s words. Maybe it was fate, maybe it was random chance.... I’ll never know But, Tim Misny helped me have the confidence and determination that was necessary to be where I’m at today. I’ve been a law enforcement officer for over 16 years. I’ve told this story to many of my coworkers.
Tim, you’ll never understand how your words that spring day helped shape my future. Your words enabled me to provide a great life for myself and my family. I’m forever grateful.
Mike


The personal attention and clarity of the matter and specifics, gave me a state of comfort and satisfaction that I could have found nowhere else! I will be forever grateful to have Tim Misny as my attorney and my friend!
I am a businessman in the Greater Cleveland area and have directed various members of my staffs as well as personal friends to Tim for solutions to their personal injury case needs. All my referrals have been more than pleased with the service and personal treatment they have received from Tim and his staff.
I strongly recommend Tim Misny and his associates should you ever need the finest legal services available in Ohio! Trust is his number one priority, trust in knowing that you will be his client second, his friend first!
