Uterine Rupture Attorney
Uterine Rupture Caused by Childbirth
Childbirth is a natural event, but it can be dangerous for both mother and baby because complications can occur. One deadly complication is a uterine rupture.
During childbirth, a woman’s uterus can experience a strain that can cause it to tear. In some cases a complete uterine rupture can result. This can occur despite the best efforts of the doctors or other medical professionals. However, uterine ruptures may be caused by negligence or medical malpractice on the part of obstetricians, surgeons, or other medical professionals.
If a doctor uses the incorrect instruments during labor or delivery, or discounts the warning signs of an impending rupture and one occurs, the physician may be found negligent and held accountable.
Suffering a ruptured uterus can be devastating, and even life threatening. It causes extreme pain to the mother, and can lead to a possible birth injury to the child during a vaginal birth. Sadly, ruptures are often due to medical malpractice. If you or a family member experienced a uterine rupture as a result of negligence, you must be fairly compensated. Call me today, and I’ll Make Them Pay!®
Symptoms That May Indicate a Uterine Rupture May Occur
Before a uterine rupture occurs, certain symptoms may indicate potential issues with the pregnancy or labor. These symptoms can serve as warning signs for you and your healthcare providers. Keep in mind that a uterine rupture is a rare event, and these symptoms are not definitive proof of rupture, but they should prompt immediate medical attention. Symptoms may include:
Abdominal Pain
Sudden, severe abdominal pain that doesn’t lessen with rest or position changes can be a sign of a uterine rupture. This pain may feel sharp, intense, and different from regular labor contractions.
Vaginal Bleeding
If you experience heavy vaginal bleeding that is bright red and not associated with the normal bloody show of labor, it could indicate a serious problem such as placental abruption or uterine rupture.
Abnormal Contractions
Contractions that are excessively strong, prolonged, or close together may be a sign of uterine hyperstimulation, which can increase the risk of rupture.
Fetal Distress
If the baby’s heart rate drops significantly or becomes irregular, it could signal distress and a potential problem with the uterus or placenta. Fetal distress could possibly lead to hypoxic ischemic encephalopathy (HIE), leading to neurological development issues.
Change in Fetal Movement
A sudden decrease or absence of fetal movement could indicate fetal distress, potentially related to uterine issues.
Abnormal Abdominal Shape
An abnormally shaped or distorted abdomen, sometimes described as a “funnel-shaped” appearance, might indicate a uterine rupture.
Unexplained Anxiety
Some individuals report a sense of impending doom or heightened anxiety before a uterine rupture occurs.
Pressure or Bulging
A sensation of pressure or bulging in the abdominal area could suggest a weakening or rupture of the uterine wall.
Back Pain
Persistent, severe back pain that doesn’t respond to rest or position changes might be associated with uterine issues.
Nausea and Vomiting
Persistent nausea and vomiting, especially if accompanied by other symptoms, could be a sign of a serious complication like uterine rupture.
Palpable Fetal Parts
Feeling a fetal limb, head, or body part through the abdominal wall could indicate that the baby has moved through a uterine tear.
Hemodynamic Changes
Rapid heart rate, low blood pressure, or signs of shock may develop due to internal bleeding associated with uterine rupture.
Although many of these signs signs and symptoms can be caused by something else, it is important that your doctor keeps an eye on the health of your uterus. Uterine ruptures occur when doctors ignore the symptoms, and that’s medical malpractice. If this has happened to you, it is important to call me. I’ll Make Them Pay!®
Potential Consequences of a Uterine Rupture
Maternal Hemorrhage
Uterine rupture, involving the tearing of blood vessels within the uterine wall, can lead to significant bleeding. This rapid blood loss poses a critical risk to the mother’s health, potentially resulting in shock—an extreme drop in blood pressure that can lead to organ failure. Immediate medical attention is crucial to control bleeding, administer blood transfusions, and perform surgical interventions to prevent life-threatening complications.
Fetal Distress
A uterine rupture disrupts the normal blood supply to the fetus, leading to a situation of fetal distress. Oxygen deprivation due to compromised blood flow can result in changes in the fetal heart rate, decreased fetal movement, and a distressed overall condition. Rapid intervention, often through an emergency cesarean section, becomes necessary to ensure the immediate delivery of the baby and mitigate potential harm.
Placental Abruption
The occurrence of uterine rupture can lead to the abrupt separation of the placenta from the uterine wall—known as placental abruption. This separation results in bleeding between the placenta and the uterine wall, which can pose severe risks to the mother and the baby. The combination of bleeding, potential oxygen deprivation, and associated complications necessitates immediate medical attention and often requires urgent delivery.
Internal Organ Damage
The tearing of the uterine wall during rupture can extend to adjacent organs such as the bladder or intestines. This damage can lead to internal bleeding, infection, and potential long-term complications. Surgical repair is often required to address the damage and prevent further adverse effects on the mother’s health.
Infection
Uterine rupture creates a direct communication between the uterine cavity and the abdominal cavity, increasing the risk of infection. Bacteria can enter the bloodstream or abdominal cavity, leading to conditions such as endometritis (uterine infection) or peritonitis (inflammation of the abdominal lining). Swift intervention, including antibiotics and possible surgical drainage, is crucial to manage and prevent the spread of infection.
Maternal Shock
Severe bleeding resulting from uterine rupture, combined with fluid loss and potential organ damage, can lead to maternal shock. Shock is a life-threatening condition characterized by a dramatic drop in blood pressure and inadequate blood flow to vital organs. Immediate resuscitation, fluid replacement, and other medical interventions are essential to stabilize the mother’s condition and prevent organ failure.
Neonatal Brain Damage or Death
Uterine rupture’s impact on fetal oxygen supply can lead to hypoxia (inadequate oxygen supply) or anoxia (complete lack of oxygen). This oxygen deprivation can result in severe consequences for the baby, including brain damage, developmental impairments, or even neonatal death. Action needs to be taken, often involving emergency delivery, and is necessary to mitigate these potential long-lasting effects.
Hysterectomy
In severe cases of uterine rupture with uncontrollable bleeding, a hysterectomy (removal of the uterus) might be the only way to save the mother’s life. This decision has profound implications for the mother’s future fertility and overall health, as well as emotional well-being.
Long-Term Physical and Emotional Consequences
Survivors of uterine rupture may experience physical complications such as adhesions (scar tissue) formation, which can affect future pregnancies and overall health. The emotional trauma of a uterine rupture can also have enduring effects on the mental well-being of both the mother and her family, requiring appropriate psychological support.
Maternal Mortality
In extreme cases, if uterine rupture is not promptly identified and managed, it can lead to maternal death due to severe hemorrhage, shock, or other complications. Rapid diagnosis and intervention are essential to prevent this tragic outcome.
Postpartum Anemia
The excessive bleeding associated with uterine rupture can lead to postpartum anemia in the mother. Anemia, characterized by low red blood cell count and reduced oxygen-carrying capacity, requires medical intervention to manage and treat, potentially involving blood transfusions and iron supplementation.
Shock Caused by Lack of Body Fluids (Hypovolemic Shock)
Severe bleeding from uterine rupture can lead to hypovolemic shock, a condition in which the body lacks sufficient fluids to maintain normal circulation. This can cause organ failure, resulting in severe consequences if not addressed promptly through fluid replacement and other supportive measures.
Bladder Injuries
The tearing of the uterine wall can cause damage to adjacent structures, including the bladder. Bladder injuries can lead to urinary complications, necessitating surgical repair and careful monitoring to prevent long-term issues.
All of these consequences are devastating, and doctors need to be aware of the uterine rupture risk factors. I have a long history of taking on medical malpractice cases, and I’ll Make Them Pay!®
Medical Professional’s Negligence
Medical professional negligence that leads to a uterine rupture can have serious and devastating consequences for both the mother and the baby. Negligence refers to a breach of the duty of care that medical professionals owe to their patients. Here are some scenarios in which medical professional negligence could potentially contribute to a uterine rupture:
Improper Management of Labor
Medical professionals have a duty to carefully monitor the progress of labor and ensure that contractions are within safe limits. If a healthcare provider fails to appropriately monitor and manage labor, excessive use of uterine stimulants like oxytocin or mismanagement of induced or augmented labor can result in overly strong and prolonged contractions. This can weaken the uterine wall and increase the risk of rupture.
Inadequate Surgical Technique
During a cesarean section or other uterine surgeries, proper surgical techniques are essential to ensure the integrity of the uterine wall. Negligent surgical practices, such as improper suturing or inadequate closure of the uterine incision, can weaken the uterine tissue and contribute to future ruptures during subsequent pregnancies or labor.
Failure to Recognize Risk Factors
Medical professionals are responsible for identifying and addressing risk factors that may increase the likelihood of uterine rupture. Neglecting to consider a patient’s medical history, previous uterine surgeries, or other risk factors can lead to inadequate precautions being taken, thus increasing the risk of rupture during labor.
Lack of Informed Consent
Medical professionals must adequately inform patients about potential risks associated with certain medical interventions. If a healthcare provider fails to provide proper informed consent—explaining the risks, benefits, and alternatives of procedures like induced labor or uterine stimulant use—patients may unknowingly agree to treatments that increase the risk of uterine rupture.
Failure to Respond to Warning Signs
Uterine rupture often presents with warning signs such as severe abdominal pain, abnormal contractions, and fetal distress. Doctors and nurses have a duty to promptly recognize and respond to these signs. If a healthcare provider fails to act swiftly upon these indications, the delay in appropriate medical intervention can lead to the worsening of the rupture and its consequences.
Inadequate Staffing or Training
Healthcare facilities must maintain adequate staffing levels and ensure that medical professionals are properly trained to handle emergency situations. Insufficient staffing or a lack of training can lead to delayed responses and inadequate care in the event of a uterine rupture.
Misinterpretation of Diagnostic Tests
Diagnostic tests such as fetal heart rate monitoring and ultrasound are crucial for assessing the well-being of both the mother and the baby during labor. Misinterpreting or disregarding these test results can lead to missed signs of distress and a failure to address the risk of rupture.
Negligent Follow-Up Care
After previous uterine surgeries, proper follow-up care is essential to monitor the healing and integrity of the uterine wall. Neglecting to provide appropriate follow-up care can lead to undetected issues that increase the risk of rupture during subsequent pregnancies.
I’ll Make Them Pay!®
Did you suffer a uterine rupture? Did a loved one die during childbirth because of a uterine rupture? If you believe medical malpractice or neglect by a physician or medical professional was to blame, I can help you. Call me today and we’ll discuss your case and “I’ll Make Them Pay!®.”
ASK TIM A QUESTION
NO COST TO YOU!
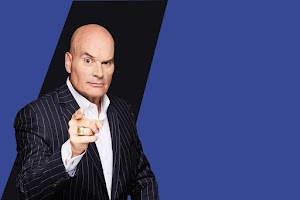
There's the Tim Misny you see on the billboards and on TV, but there's another Tim Misny that I know up close and personal.
The Tim Misny I know is genuinely passionate about helping the hard working little folks who get pushed around the big folks. He actually, really honestly cares about people who run into bad luck at no fault of their own. Tim has quietly, out of the sight of cameras and with no fanfare shared generously with the marginalized in our society; single moms, Veterans and others without expecting anything in return.
He calls them like he sees them and you wouldn't want to take your troubles to anyone else.
Thank you Tim for being a light in this community!
City, State and Above State Level Situation .
Pro Se !
Thank you Tim
father figure one day. Tim loves nature & shares the true beauty of nature with how he raises his kids. From biking through trails & having his kids learn how to nurture the family garden - he teaches valuable lessons on how to appreciate the world we live in. I know that Tim is just a phone call away & always urgent to responding no matter the situation. He has given me some of the greatest advice & continously throwing positive energy my way! I'm honored to know him & be a friend of his. He is the true practioneer of changing lives & paying it forward. He has taught me so much in just a short amount of time. Tim Misny, a man that wakes up every single day to make a difference!

After I helped him through the checkout and he left, many different employees at the garden center asked me if I knew who that man was. I did not. They told me, “That’s Tim Misny!” Once I figured out “who” Tim Misny was, my confidence grew. It was a pivotal moment. One in which steered the rest of my life. His words stuck with me. I worked hard and obtained my Associate’s Degree in Criminal Justice. I was hired by a local Law Enforcement Agency at the age of 21. I was sent to the Ohio State Highway Patrol Academy, which was an extremely tough place to be, to say the least. At the Academy, they try to break those who don’t have a determined spirit. On days I wanted to quit, I remembered Tim’s words. Maybe it was fate, maybe it was random chance.... I’ll never know But, Tim Misny helped me have the confidence and determination that was necessary to be where I’m at today. I’ve been a law enforcement officer for over 16 years. I’ve told this story to many of my coworkers.
Tim, you’ll never understand how your words that spring day helped shape my future. Your words enabled me to provide a great life for myself and my family. I’m forever grateful.
Mike


The personal attention and clarity of the matter and specifics, gave me a state of comfort and satisfaction that I could have found nowhere else! I will be forever grateful to have Tim Misny as my attorney and my friend!
I am a businessman in the Greater Cleveland area and have directed various members of my staffs as well as personal friends to Tim for solutions to their personal injury case needs. All my referrals have been more than pleased with the service and personal treatment they have received from Tim and his staff.
I strongly recommend Tim Misny and his associates should you ever need the finest legal services available in Ohio! Trust is his number one priority, trust in knowing that you will be his client second, his friend first!
